Young adult cancer. Myth or Realty?
- netmd
- 29 de abril de 2024
- Oncología Médica
- 0 Comments
- Adrian P. Huñis MD
- School of Medicine
- Universidad de Buenos Aires
- Emeritus Member of ASCO
- Emeritus Member of ESMO
- Honorary Member of the AMA
Introduction
Young Adult Cancer (YAC) is a reality, not a myth. More and more young adults are being diagnosed with cancer. While cancer has traditionally been associated with older individuals, the incidence of cancer in young adults is on the rise due to factors such as lifestyle, genetics, and exposure to environmental carcinogens.
It is important to raise awareness among this population about the importance of early detection, timely treatment, and emotional support during the illness. Despite the challenges faced by young adults with cancer, there are resources and organizations dedicated to supporting them in their battle against the disease. Therefore, young adult cancer is a reality that should not be ignored.
Who is defined as a “young adult?”
A young adult is generally defined as an individual between the ages of 18 and 39 years old. This age range is often characterized by significant life transitions, such as completing education, starting a career, establishing independence, and forming long-term relationships. Young adults in this age group may also be in the process of exploring their identity, values, and goals for the future. Additionally, young adults may face unique challenges and experiences related to their stage of life, including health concerns, financial responsibilities, and societal expectations.
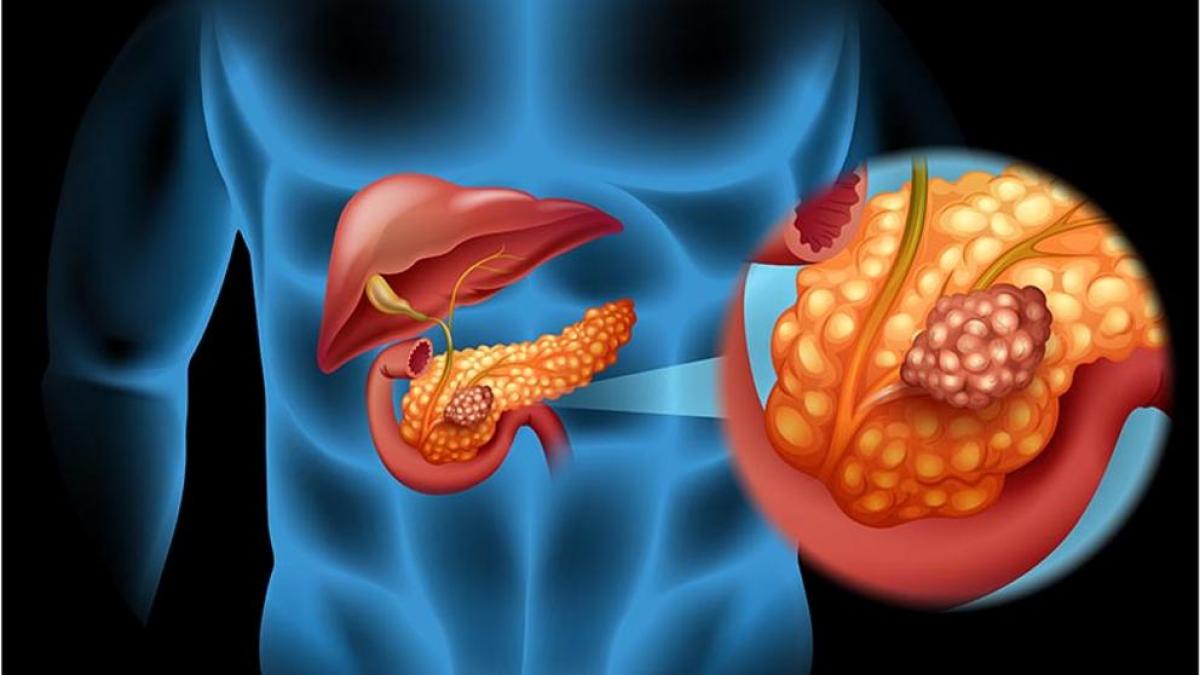
Some of the most commonly diagnosed tumors in young adults include:
- Breast cancer
- Testicular cancer
- Melanoma (skin cancer)
- Thyroid cancer
- Colorectal cancer
- Hodgkin lymphoma
- Non-Hodgkin lymphoma
- Cervical cancer
- Ovarian cancer
- Brain tumors
Some of the most commonly diagnosed tumors in young adults.
These are just a few examples of the types of tumors that can be diagnosed in young adults. It is important for young adults to be aware of their risk factors, symptoms, and screening guidelines for early detection and treatment of these cancers.
Some of the tumors that are commonly diagnosed in young adults include various types of cancer that can affect different organs and systems in the body. Breast cancer is one of the most common cancers in young women, while testicular cancer is more frequently diagnosed in young men. Melanoma, a type of skin cancer, can also affect young adults, especially those with a history of sun exposure or indoor tanning.
Thyroid cancer, colorectal cancer, and various types of lymphoma are also among the tumors that can occur in young adults. Cervical cancer and ovarian cancer are specific to female reproductive organs and can affect young women in their reproductive years. Brain tumors, although less common, can also be diagnosed in young adults and may present unique challenges due to their location and potential impact on cognitive function.
It is important for young adults to be aware of the signs and symptoms of these tumors, as well as any risk factors that may increase their likelihood of developing cancer. Early detection through regular screenings and prompt medical intervention can improve outcomes and quality of life for young adults diagnosed with cancer.
What is the explanation of this phenomenon?
The increasing incidence of cancer in young adults can be attributed to a combination of genetic, environmental, and lifestyle factors. While cancer has traditionally been associated with older individuals, there are several reasons why cancer is now being diagnosed more frequently in young adults:
- Genetic predisposition: Some individuals may have genetic mutations that increase their risk of developing cancer at a younger age. These mutations can be inherited or acquired over time and can predispose individuals to certain types of cancer.
- Environmental factors: Exposure to carcinogens in the environment, such as tobacco smoke, air pollution, radiation, and certain chemicals, can increase the risk of developing cancer at any age. Young adults may be exposed to these carcinogens through their occupation, lifestyle choices, or living environment.
- Lifestyle factors: Unhealthy lifestyle choices, such as poor diet, lack of exercise, excessive alcohol consumption, and smoking, can contribute to the development of cancer in young adults. These factors can impact overall health and increase the risk of cancer development.
- Delayed diagnosis: Young adults may not be as vigilant about their health or may not seek medical attention for symptoms that could indicate cancer. This can result in delays in diagnosis and treatment, allowing the cancer to progress to a more advanced stage.
- Changing disease patterns: The overall landscape of cancer is evolving, with some types of cancer becoming more prevalent in younger populations. Factors such as changing dietary habits, environmental pollution, and increased exposure to risk factors may contribute to this shift.
Overall, the increase in cancer diagnoses among young adults is a complex phenomenon influenced by a combination of genetic, environmental, and lifestyle factors. It underscores the importance of awareness, early detection, and prevention strategies for reducing the impact of cancer on this population.
Genetic profile
Young adults who are diagnosed with cancer may have a variety of genetic profiles that contribute to their increased risk of developing the disease at a younger age. Some common genetic characteristics and profiles seen in young cancer patients include:
- Inherited genetic mutations: Some young adults may carry inherited genetic mutations, such as BRCA1 and BRCA2 mutations for breast and ovarian cancer, Lynch syndrome for colorectal and other cancers, or mutations in genes associated with hereditary forms of melanoma or thyroid cancer.
- Acquired genetic mutations: Young adults may also develop cancer as a result of acquired genetic mutations that occur due to exposure to carcinogens, environmental factors, or lifestyle choices. These mutations can drive the development and progression of cancer in these individuals.
- Genetic instability: Some young adults may have genetic instability or a higher rate of genetic mutations, which can increase their susceptibility to developing cancer at a younger age. This genetic instability may be influenced by various factors, including DNA repair mechanisms and environmental exposures.
- Tumor suppressor gene mutations: Mutations in tumor suppressor genes, which normally help regulate cell growth and prevent cancer development, can predispose young adults to certain types of cancer. Examples include mutations in the TP53 gene associated with Li-Fraumeni syndrome or mutations in the RB1 gene linked to retinoblastoma and other cancers.
- Epigenetic changes: Epigenetic modifications, which can alter gene expression without changing the underlying DNA sequence, may also play a role in the development of cancer in young adults. Changes in DNA methylation, histone modifications, and microRNA expression patterns can affect gene regulation and contribute to cancer risk.
Young adults with cancer may have a range of genetic factors that influence their susceptibility to the disease. Understanding these genetic profiles can help guide personalized treatment approaches, genetic counseling, and risk assessment for individuals at risk for developing cancer at a young age.
Molecular alterations
Young adults with cancer may exhibit various molecular alterations that contribute to the development and progression of the disease. Some common molecular alterations seen in these patients include:
- Mutations in oncogenes: Oncogenes are genes that, when mutated or overexpressed, can promote cell growth and division, leading to cancer. Young adults with cancer may harbor mutations in oncogenes such as KRAS, EGFR, BRAF, or HER2, which can drive tumor growth and resistance to treatment.
- Mutations in tumor suppressor genes: Tumor suppressor genes help regulate cell growth and prevent the development of cancer. Mutations in tumor suppressor genes such as TP53, PTEN, or RB1 can disrupt normal cellular functions and contribute to the development of cancer in young adults.
- Chromosomal abnormalities: Chromosomal aberrations, such as translocations, deletions, amplifications, or rearrangements, can result in the activation of oncogenes or the inactivation of tumor suppressor genes. These chromosomal abnormalities can drive cancer development and progression in young adult patients.
- Epigenetic modifications: Epigenetic changes, including DNA methylation, histone modifications, and microRNA dysregulation, can alter gene expression patterns in cancer cells. Young adults with cancer may exhibit epigenetic alterations that impact key cellular processes and contribute to tumor growth and metastasis.
- Microsatellite instability: Microsatellite instability (MSI) is a molecular marker of genetic instability that can be found in various types of cancer. Young adults with MSI-high tumors may have an increased risk of developing cancer and may respond differently to certain treatments, such as immune checkpoint inhibitors.
- Gene fusions: Gene fusions involve the abnormal fusion of two separate genes, resulting in the creation of a novel gene with oncogenic properties. Young adults with cancer may harbor gene fusions, such as ALK or ROS1 rearrangements in lung cancer or BCR-ABL fusion in leukemia, which can drive tumor growth and serve as therapeutic targets.
The molecular landscape of cancer in young adults is diverse and complex, with a wide range of molecular alterations contributing to the disease. Understanding these molecular changes can help guide treatment decisions, identify targeted therapies, and improve outcomes for young adult cancer patients.
Role of lifestyle
Lifestyle factors play a significant role in the development and progression of cancer in young adults. Several studies have shown that behaviors such as smoking, poor diet, lack of physical activity, excess alcohol consumption, and exposure to environmental toxins can increase the risk of cancer in this population. Additionally, maintaining a healthy lifestyle that includes regular exercise, a balanced diet, limited alcohol intake, and avoidance of tobacco can help reduce the risk of developing cancer and improve outcomes for young adults diagnosed with the disease. Therefore, lifestyle choices are crucial in cancer prevention and management in young adults.
The impact of lifestyle on cancer risk and outcomes in young adults cannot be overstated. Numerous studies have demonstrated the profound influence of lifestyle factors on the development and progression of cancer in this population.
One of the most well-established lifestyle factors associated with cancer risk is smoking. Tobacco use is a leading cause of various types of cancer, including lung, throat, and bladder cancer. Young adults who smoke are at a significantly higher risk of developing these and other types of cancer compared to non-smokers. Additionally, exposure to secondhand smoke can also increase the risk of cancer in this age group.
Diet and nutrition are also critical determinants of cancer risk in young adults. A diet high in processed foods, red and processed meats, sugary beverages, and saturated fats has been linked to an increased risk of cancer. Conversely, a diet rich in fruits, vegetables, whole grains, and lean proteins has been associated with a reduced risk of cancer. Maintaining a healthy weight through proper nutrition and regular physical activity is essential for cancer prevention in young adults.
Alcohol consumption is another lifestyle factor that can influence cancer risk in young adults. Excessive alcohol intake has been linked to an increased risk of several types of cancer, including breast, liver, and esophageal cancer. Limiting alcohol consumption and following recommended guidelines for moderate drinking can help reduce the risk of cancer in this age group.
Physical activity is also a key component of a healthy lifestyle that can impact cancer risk and outcomes in young adults. Regular exercise has been shown to reduce the risk of developing certain types of cancer, including breast, colon, and endometrial cancer. Exercise can also improve treatment outcomes and quality of life for young adults diagnosed with cancer.
In addition to these lifestyle factors, environmental exposures and occupational hazards can also contribute to cancer risk in young adults. Exposure to carcinogens in the workplace or environmental pollutants in the air, water, or soil can increase the risk of cancer development. Taking steps to minimize exposure to these risks through proper safety measures and environmental regulations is essential for cancer prevention in young adults.
In conclusion, lifestyle choices play a crucial role in determining cancer risk and outcomes in young adults. Adopting healthy behaviors such as avoiding tobacco, following a balanced diet, limiting alcohol intake, staying physically active, and minimizing exposure to environmental toxins can help reduce the risk of cancer and improve overall health in this population. Education and awareness about the impact of lifestyle on cancer risk are essential for empowering young adults to make informed choices that promote their well-being and reduce their cancer risk.
- A) Tobacco:
There is a well-established link between tobacco use and an increased risk of cancer. Smoking has been identified as a major cause of various types of cancer, including lung, throat, and bladder cancer. The chemicals in tobacco smoke can damage DNA and lead to the development of cancerous cells. According to the Centers for Disease Control and Prevention (CDC), smoking is responsible for approximately 30% of all cancer deaths in the United States. Numerous scientific studies have provided strong evidence of the association between tobacco use and cancer incidence, highlighting the importance of tobacco cessation in reducing the risk of cancer in young adults.
- B) Diet:
The role of diet in cancer risk has been extensively studied, and there is compelling evidence that a healthy diet can help reduce the risk of cancer. A diet high in fruits, vegetables, whole grains, and lean proteins has been associated with a lower risk of various types of cancer, while a diet high in processed foods, red and processed meats, and sugary beverages has been linked to an increased risk of cancer. The World Cancer Research Fund estimates that up to one-third of cancer cases may be preventable through dietary and lifestyle changes. Numerous research studies have demonstrated the impact of diet on cancer risk, underscoring the importance of a balanced and nutritious diet in cancer prevention among young adults.
- C) Physical Activity:
Regular physical activity has been shown to reduce the risk of cancer and improve overall health. Exercise can help maintain a healthy weight, boost the immune system, and reduce inflammation, all of which contribute to lowering cancer risk. The American Cancer Society recommends at least 150 minutes of moderate-intensity exercise per week to reduce the risk of cancer. Research studies have consistently demonstrated the beneficial effects of physical activity on cancer prevention, with some studies suggesting that regular exercise may reduce the risk of certain types of cancer by up to 20-30%.
- D) Alcohol:
Excessive alcohol consumption has been linked to an increased risk of several types of cancer, including breast, liver, and esophageal cancer. Alcohol can damage DNA, increase inflammation, and impair the body’s ability to repair damaged cells, all of which can contribute to the development of cancer. The International Agency for Research on Cancer (IARC) has classified alcohol as a Group 1 carcinogen, indicating that it is a known cause of cancer in humans. Numerous epidemiological studies have provided strong evidence of the association between alcohol consumption and cancer risk, emphasizing the importance of moderation or abstinence in reducing cancer risk.
Cancer in young adults can be more aggressive?
There is evidence to suggest that cancer in young adults can be more aggressive and have a worse prognosis compared to cancer in older adults. Several factors contribute to this phenomenon.
Firstly, young adults may have different types of cancer that are inherently more aggressive, such as certain types of leukemia or sarcomas. These cancers often have a higher rate of metastasis and resistance to treatment, leading to poorer outcomes.
Secondly, young adults may be diagnosed at a later stage of the disease, as symptoms can be overlooked or attributed to other causes in this age group. Delayed diagnosis can result in the cancer being more advanced at the time of treatment, making it harder to eradicate.
Additionally, young adults may have unique challenges in cancer treatment, such as fertility preservation concerns and the impact of treatment on long-term quality of life. These factors can complicate treatment decisions and may affect overall prognosis.
However, it is important to note that each individual case of cancer is unique, and prognosis can vary widely depending on factors such as cancer type, stage at diagnosis, genetic profile, and response to treatment. Early detection, personalized treatment approaches, and comprehensive care can all contribute to improved outcomes for young adults with cancer. Ongoing research and advancements in cancer care continue to improve the prognosis for all age groups affected by cancer.
Prevention and treatment
- A) Prevention:
From a prevention standpoint, several strategies are being implemented to reduce the incidence of cancer among young adults. These include public health campaigns promoting healthy lifestyle choices, such as tobacco cessation programs, healthy eating initiatives, and physical activity promotion. Additionally, efforts are being made to increase cancer screening rates among young adults to detect cancer at an earlier, more treatable stage. Educational programs are also being developed to raise awareness about cancer risk factors and the importance of early detection. Research into innovative prevention strategies, such as vaccination against cancer-causing viruses like HPV, is ongoing to further reduce the burden of cancer among young adults.
- B) Treatment:
In terms of treatment for cancer among young adults, there have been significant advancements in recent years. Personalized medicine approaches, such as targeted therapies and immunotherapy, are being increasingly used to tailor treatment plans to an individual’s specific cancer type and genetic profile. These precision medicine techniques have shown promising results in improving treatment outcomes and reducing side effects. Additionally, advancements in surgical techniques, radiation therapy, and supportive care have improved survival rates and quality of life for young adults undergoing cancer treatment.
Multidisciplinary care teams, including oncologists, surgeons, radiologists, and supportive care specialists, collaborate to provide comprehensive treatment plans that address the physical, emotional, and psychosocial needs of young adult cancer patients. Clinical trials are also playing a vital role in testing novel treatment approaches and identifying new therapies that may benefit young adults with cancer.
Furthermore, survivorship programs are being developed to support young adult cancer survivors in managing the long-term effects of cancer treatment, such as fertility issues, cognitive impairment, and emotional well-being. These programs focus on survivorship care planning, monitoring for late effects of treatment, and providing resources for physical and psychological support.
A holistic approach to cancer care that encompasses prevention, early detection, personalized treatment, and survivorship support is crucial in addressing the unique needs of young adults affected by cancer. Ongoing research, advocacy efforts, and healthcare initiatives are aimed at improving outcomes and quality of life for this vulnerable population.
The treatment approach for cancer in young adults may differ from that in older adults due to a variety of factors, including the type of cancer, the patient’s overall health and medical history, and the individual’s preferences and goals for treatment.
In some cases, young adults may receive more aggressive treatment regimens compared to older adults, especially if the cancer is more aggressive or advanced at the time of diagnosis. This could involve a combination of surgery, chemotherapy, radiation therapy, targeted therapy, immunotherapy, or other novel treatment approaches.
Additionally, young adults may be more likely to undergo fertility preservation procedures before starting cancer treatment, as preserving fertility is often a significant concern for this age group. This may involve techniques such as egg or sperm freezing, embryo freezing, or ovarian tissue preservation, depending on the individual’s circumstances and treatment plan.
Young adults may also be more likely to participate in clinical trials or receive personalized or targeted therapies based on the specific characteristics of their cancer, such as genetic mutations or biomarkers that can guide treatment decisions. These precision medicine approaches can help tailor treatment to the individual’s unique cancer biology and potentially improve outcomes.
Furthermore, young adults may benefit from psychosocial support services, survivorship care planning, and resources specifically designed for their age group to address the emotional, social, and practical challenges that can arise during and after cancer treatment.
The treatment of cancer in young adults is often multidisciplinary and individualized, taking into account the specific needs and preferences of the patient. Collaboration between oncologists, surgeons, radiation oncologists, fertility specialists, mental health professionals, and other healthcare providers is essential to provide comprehensive care and support throughout the cancer treatment journey.
Future
It is difficult to predict with certainty how the treatment approach for cancer in young adults will evolve over the next ten years. However, based on current trends and advancements in cancer research and treatment, several potential developments can be anticipated.
- Personalized Medicine: There is a growing emphasis on personalized medicine in cancer treatment, which aims to tailor therapies based on the individual characteristics of the patient and their cancer. Advances in genomic sequencing and biomarker testing may lead to more targeted and effective treatments for young adults with cancer.
- Immunotherapy: Immunotherapy has emerged as a promising treatment approach for various types of cancer, including some that are more common in young adults. Over the next decade, further research and clinical trials may expand the use of immunotherapy in the treatment of young adult cancers, potentially improving outcomes and reducing side effects.
- Fertility Preservation: Continued advancements in fertility preservation techniques may offer more options for young adults facing cancer treatment. Research in areas such as ovarian tissue transplantation, artificial reproductive technologies, and oncofertility may provide new opportunities for preserving fertility in cancer patients.
- Survivorship Care: There is a growing recognition of the importance of survivorship care in cancer treatment, particularly for young adults who may face unique long-term health and psychosocial challenges. In the next decade, there may be increased focus on developing comprehensive survivorship care plans and resources tailored to the needs of young adult cancer survivors.
- Access to Clinical Trials: Efforts to increase access to clinical trials and novel treatment approaches for young adults with cancer are likely to continue. Collaborations between academic institutions, research organizations, and industry partners may lead to more opportunities for young adults to participate in cutting-edge research and potentially benefit from innovative therapies.
The next years holds the promise of continued advancements in cancer treatment, with a focus on personalized, targeted therapies, improved survivorship care, and increased access to innovative treatments for young adults with cancer. Collaboration among healthcare providers, researchers, and patient advocacy groups will be essential in driving progress and improving outcomes for young adults facing a cancer diagnosis.
Conclusion
In conclusion, the landscape of cancer treatment for young adults is expected to undergo significant advancements and improvements over the next ten years. The shift towards personalized medicine, with a focus on tailored therapies based on individual patient characteristics and cancer profiles, holds great promise for improving treatment outcomes and reducing side effects. The continued development and expansion of immunotherapy as a treatment approach for various types of cancer, including those more prevalent in young adults, may further enhance the options available for patients.
Additionally, the advancement of fertility preservation techniques and oncofertility research may offer young adult cancer patients more opportunities to preserve their fertility and family-building options during and after treatment. The recognition of the importance of survivorship care, with a focus on addressing the long-term health and psychosocial needs of young adult cancer survivors, is likely to drive the development of comprehensive survivorship care plans and resources tailored to this population.
Efforts to increase access to clinical trials and novel treatment approaches for young adults with cancer are expected to continue, providing opportunities for patients to benefit from cutting-edge research and therapies. Collaborations among healthcare providers, researchers, industry partners, and patient advocacy groups will be crucial in driving progress and improving outcomes for young adults facing a cancer diagnosis.
The next decade holds great potential for advancements in cancer treatment for young adults, with a focus on personalized, targeted therapies, improved survivorship care, enhanced fertility preservation options, and increased access to innovative treatments. These developments have the potential to significantly impact the lives of young adult cancer patients, offering hope for improved outcomes and quality of life in the years to come.
The landscape of cancer treatment for young adults is poised for significant advancements and improvements in the coming years. The shift towards personalized medicine, with an emphasis on tailoring treatments based on individual patient characteristics and cancer profiles, is a promising development that has the potential to revolutionize the way cancer is treated in this population. By utilizing genomic profiling, biomarker testing, and other advanced technologies, healthcare providers can better understand the underlying biology of each patient’s cancer and tailor treatment plans to target specific molecular abnormalities, leading to more effective and less toxic therapies.
The continued evolution and expansion of immunotherapy as a treatment modality for various types of cancer, including those commonly diagnosed in young adults, represent a groundbreaking advancement in the field. Immunotherapy has shown remarkable success in some patients, offering the possibility of durable responses and improved survival outcomes. As ongoing research uncovers new immunotherapy targets and refines treatment strategies, the potential for expanding the use of these novel therapies in young adult cancer patients continues to grow.
Furthermore, the field of oncofertility, which focuses on preserving fertility in cancer patients, is rapidly advancing, offering young adults facing cancer diagnoses more options to protect their reproductive potential. By integrating fertility preservation techniques into the initial treatment planning process, healthcare providers can help young adult cancer patients make informed decisions about their future fertility options, improving their quality of life and overall well-being.
In addition, the recognition of the unique needs of young adult cancer survivors is driving the development of specialized survivorship care programs tailored to this population. Addressing the long-term physical, emotional, and psychosocial effects of cancer treatment is essential for promoting the health and well-being of survivors and helping them navigate the challenges of survivorship.
Collaboration among healthcare providers, researchers, industry partners, and patient advocacy groups will be critical in driving progress and innovation in the field of young adult oncology. By working together to advocate for increased access to clinical trials, novel treatment approaches, and comprehensive survivorship care, stakeholders can improve outcomes and quality of life for young adults with cancer.
The future of cancer treatment for young adults is bright, with advancements in personalized medicine, immunotherapy, oncofertility, and survivorship care offering new hope and opportunities for improved outcomes and quality of life. By continuing to prioritize research, innovation, and collaboration, we can make significant strides in addressing the unique needs of young adult cancer patients and improving their overall cancer care experience.
References
- Siegel RL, Miller KD, Jemal A. Cancer statistics, 2020. CA Cancer J Clin. 2020;70(1):7-30.
- National Cancer Institute. A snapshot of adolescent and young adult cancers. Accessed from https://www.cancer.gov/types/aya on April 15, 2021.
- Keegan TH, Ries LA, Barr RD, Geiger AM, Dahlke DV, Pollock BH, et al. Comparison of cancer survival trends in the United States of adolescents and young adults with those in children and older adults. Cancer. 2016;122(7):1009-16.
- Smith AW, Seibel NL, Lewis DR, Albritton KH, Blair DF, Blanke CD, et al. Next steps for adolescent and young adult oncology workshop: An update on progress and recommendations for the future. Cancer. 2016;122(7):988-99.
- Tricoli JV, Blair DG, Anders CK, Bleyer WA, Boardman LA, Khan J, et al. Biologic and clinical characteristics of adolescent and young adult cancers: Acute lymphoblastic leukemia, colorectal cancer, breast cancer, melanoma, and sarcoma. Cancer. 2016;122(7):1017-28.
- Zebrack B, Kent EE, Keegan TH, Kato I, Smith AW, AYA HOPE Study Collaborative Group. “Cancer sucks,” and other ponderings by adolescent and young adult cancer survivors. J Psychosoc Oncol. 2014;32(1):1-15.
- Bleyer A, Montello M, Budd T, Saxman S. National survival trends of young adults with sarcoma: Lack of progress is associated with lack of clinical trial participation. Cancer. 2005;103(9):1891-7.
- Armuand GM, Wettergren L, Rodriguez-Wallberg KA, Lampic C. Desire for children, difficulties achieving a pregnancy, and infertility distress 3 to 7 years after cancer diagnosis. Support Care Cancer. 2014;22(10):2805-12.
- Gorman JR, Bailey S, Pierce JP, Su HI. How do you feel about fertility and parenthood? The voices of young female cancer survivors. J Cancer Surviv. 2012;6(2):200-9.
- Parsons HM, Harlan LC, Lynch CF, Hamilton AS, Wu XC, Kato I, et al. Impact of cancer on work and education among adolescent and young adult cancer survivors. J Clin Oncol. 2012;30(19):2393-400.
- 11. Zebrack BJ, Casillas J, Nohr L, Adams H, Zeltzer Fertility issues for young adult survivors of childhood cancer. Psychooncology. 2004;13(10):689-99.
- 1 Quinn GP, Vadaparampil ST, Gwede CK, Miree C, King LM, Clayton HB, et al. Discussion of fertility preservation with newly diagnosed patients: Oncologists’ views. J Cancer Surviv. 2007;1(2):146-55.
- 1 Oktay K, Harvey BE, Partridge AH, Quinn GP, Reinecke J, Taylor HS, et al. Fertility preservation in patients with cancer: ASCO clinical practice guideline update. J Clin Oncol. 2018;36(19):1994-2001.
- 1 Armuand GM, Rodriguez-Wallberg KA, Wettergren L, Ahlgren J, Enskär K, Lampic C. Desire for children, difficulties achieving a pregnancy, and infertility distress 3 to 7 years after cancer diagnosis. Support Care Cancer. 2014;22(10):2805-12.
- Zebrack B, Kent EE, Keegan TH, Kato I, Smith AW, AYA HOPE Study Collaborative Group. “Cancer sucks,” and other ponderings by adolescent and young adult cancer survivors. J Psychosoc Oncol. 2014;32(1):1-15.
- Bleyer A, Barr R, Hayes-Lattin B, Thomas D, Ellis C, Anderson B, et al. The distinctive biology of cancer in adolescents and young adults. Nat Rev Cancer. 2008;8(4):288-98.
- 1 Warner EL, Kent EE, Trevino KM, Parsons HM, Zebrack BJ, Kirchhoff AC. Social well-being among adolescents and young adults with cancer: A systematic review. Cancer. 2016;122(7):1029-37.