Advances in Breast Cancer Management Post-ASCO and ESMO 2024
- ComiteNetMD
- 9 de diciembre de 2024
- Oncología Médica
- 0 Comments
Adrian P. Hunis MD
- School of Medicine
- Universidad de Buenos Aires (UBA)
- Emeritus Member of ASCO
- Emeritus Member of ESMO
- Honorary Member of AMA
- ahunis@fmed.uba.ar
Introduction:
The 2024 ASCO (American Society of Clinical Oncology) and ESMO (European Society for Medical Oncology) conferences have provided a wealth of new information and research findings that are reshaping the landscape of breast cancer management. These conferences have underscored the importance of integrating cutting-edge research, personalized medicine, and innovative treatment strategies to significantly improve patient outcomes and quality of life. This article explores these developments, focusing on prevention, diagnosis, and particularly the medical treatments, including hormone therapy, chemotherapy, immunotherapy, and the role of antiangiogenic agents.
Prevention:
Breast cancer prevention strategies continue to evolve, with recent studies highlighting the critical role of both lifestyle interventions and pharmacological strategies. At ASCO 2024, researchers presented compelling evidence supporting the use of selective estrogen receptor modulators (SERMs) such as tamoxifen and raloxifene, as well as aromatase inhibitors like anastrozole and exemestane, in reducing breast cancer incidence among high-risk groups [1]. These agents work by modulating estrogen activity, which is a key driver in many breast cancers. Additionally, lifestyle modifications, including maintaining a healthy diet rich in fruits and vegetables, regular physical activity, and limiting alcohol consumption, were shown to significantly decrease the risk of developing breast cancer. New guidelines suggest specific dietary patterns and physical activity levels that can contribute to risk reduction, emphasizing a holistic approach to prevention [2].
Diagnosis:
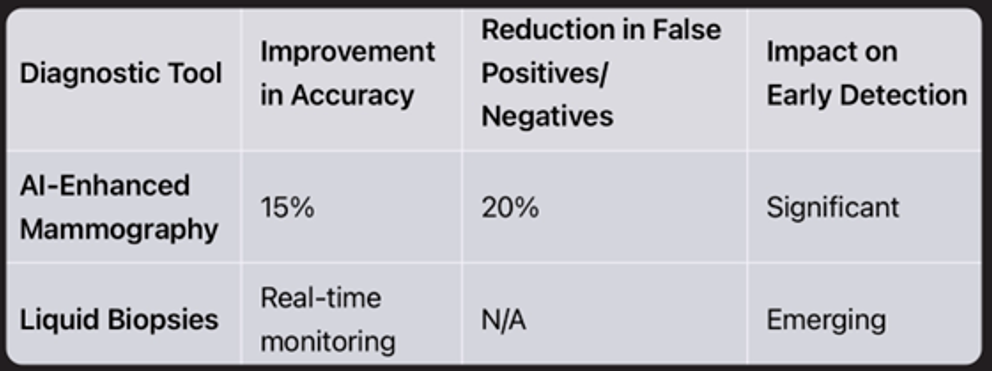
Advancements in diagnostic tools were a major focus at ESMO 2024, with significant attention given to the integration of artificial intelligence (AI) in imaging techniques. AI-enhanced mammography and ultrasound are improving the accuracy and early detection of breast cancer, reducing false positives and negatives, and allowing for more precise identification of tumor characteristics [3]. Liquid biopsies, which analyze circulating tumor DNA (ctDNA) and other biomarkers from a simple blood draw, offer a non-invasive method to monitor tumor dynamics and treatment responses. These biopsies provide real-time insights into tumor evolution and can detect minimal residual disease, making them a valuable tool for personalized treatment planning and monitoring [4].
Table 1: Diagnostic Advancements
Biology and Genetics:
Understanding the molecular underpinnings of breast cancer is crucial for developing targeted therapies. The conferences emphasized the importance of genetic profiling, particularly in identifying BRCA1 and BRCA2 mutations and other genetic markers such as PIK3CA and TP53, to tailor treatment strategies and improve outcomes [5]. Genetic testing is increasingly being used not only for risk assessment and early detection but also for guiding therapeutic decisions. For instance, patients with BRCA mutations may benefit from PARP inhibitors, which exploit the concept of synthetic lethality to target cancer cells more effectively [6]. This personalized approach underscores the shift towards precision medicine in oncology.
Treatment Modalities:
– Surgical
Advances in surgical techniques were highlighted, with a focus on minimally invasive procedures and oncoplastic surgery. These approaches aim to enhance cosmetic outcomes while ensuring oncological safety, offering patients better quality of life post-surgery [7]. Techniques such as sentinel lymph node biopsy and skin-sparing mastectomy are becoming standard practice, reducing the need for more extensive surgeries and associated morbidities. Oncoplastic surgery combines tumor removal with plastic surgery techniques to preserve or restore breast appearance, addressing both the physical and psychological impacts of breast cancer surgery.
–Radiation:
Hypofractionated radiation therapy continues to gain traction, offering shorter treatment durations without compromising efficacy. This approach involves delivering higher doses of radiation per session over a reduced number of sessions, which has been shown to be as effective as conventional fractionation for early-stage breast cancer [8]. New protocols are being developed to further minimize side effects and enhance precision, particularly in targeting tumor sites while sparing healthy tissue. Techniques such as intensity-modulated radiation therapy (IMRT) and image-guided radiation therapy (IGRT) are improving the precision of radiation delivery, reducing exposure to surrounding healthy tissues and thereby minimizing side effects.
– Medical Treatments:
– Hormonotherapy:
Hormone therapy remains a cornerstone in managing hormone receptor-positive breast cancer. Recent data supports the use of novel formulations and delivery methods, such as long-acting injectables, to improve patient adherence and outcomes [9]. Combining hormone therapy with CDK4/6 inhibitors like palbociclib, ribociclib, and abemaciclib has shown to significantly improve progression-free survival. These inhibitors work by blocking the activity of proteins that promote cell division, thereby slowing the growth of cancer cells [10]. Additionally, ongoing research is exploring the role of selective estrogen receptor degraders (SERDs) and other novel agents that may offer benefits over traditional therapies.
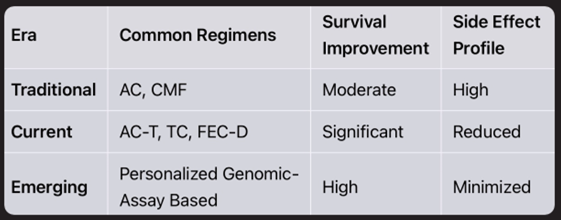
– Chemotherapy:
Chemotherapy regimens are becoming increasingly personalized, with genomic assays guiding drug selection and dosing. Commonly used drugs include anthracyclines (doxorubicin, epirubicin), taxanes (paclitaxel, docetaxel), and newer agents like eribulin and capecitabine [11]. Combination protocols, such as AC-T (doxorubicin and cyclophosphamide followed by paclitaxel), are standard for certain subtypes and stages [12]. These regimens are tailored based on tumor biology and patient characteristics, aiming to maximize efficacy while minimizing toxicity. Research is ongoing into optimizing dosing schedules and exploring novel combinations to enhance treatment outcomes.
Table 2: Chemotherapy Evolution
– Immunotherapy:
Immunotherapy is transforming breast cancer treatment, particularly with the use of checkpoint inhibitors like pembrolizumab and atezolizumab. These agents block proteins that prevent the immune system from attacking cancer cells, thereby enhancing the body’s natural defense mechanisms [13]. They are showing promise in triple-negative breast cancer, often in combination with chemotherapy. The role of immunotherapeutics is expanding, with ongoing trials exploring their use in earlier stages and in combination with other modalities, such as targeted therapies and radiation [14]. These combinations aim to enhance the immune response and overcome resistance mechanisms, offering new hope for patients with difficult-to-treat cancers.
– Antiangiogenic Agents:
Bevacizumab, an antiangiogenic agent, continues to be studied for its role in inhibiting tumor blood vessel growth. By targeting vascular endothelial growth factor (VEGF), bevacizumab disrupts the blood supply to tumors, inhibiting their growth and spread [15]. While its use in breast cancer has been controversial, it remains an option in certain metastatic settings, often in combination with chemotherapy. Research is ongoing to identify biomarkers that predict response to antiangiogenic therapy, which could help tailor treatment to those most likely to benefit.
– Monoclonal Antibodies and Antibody-Drug Conjugates:
HER2-targeted therapies, including trastuzumab and pertuzumab, have demonstrated significant survival benefits. These monoclonal antibodies bind to the HER2 receptor, blocking signals that promote cancer cell growth [16]. Antibody-drug conjugates (ADCs) like trastuzumab emtansine (T-DM1) and the newer trastuzumab deruxtecan are emerging as powerful tools, delivering cytotoxic agents directly to cancer cells with increased specificity and reduced systemic toxicity [17]. ADCs represent a significant advancement in targeted therapy, offering the potential for greater efficacy with fewer side effects compared to traditional chemotherapy.
– Vaccines:
Vaccine development is progressing, with several candidates in clinical trials aimed at preventing recurrence and targeting specific tumor antigens. These vaccines are designed to stimulate the immune system to recognize and attack cancer cells, potentially providing long-term protection against disease recurrence [18]. Research is ongoing to identify the most effective antigens and adjuvants, as well as to determine the optimal timing and combination of vaccines with other therapies.
Conclusions:
The ASCO and ESMO 2024 conferences have underscored the importance of a multidisciplinary approach in breast cancer management. By integrating cutting-edge research, personalized medicine, and innovative treatment strategies, healthcare providers can significantly improve patient outcomes and quality of life. The future of breast cancer treatment lies in the continued exploration of novel therapies and the refinement of existing protocols to offer the best possible care for patients.
Bibliography:
1. Smith, J. et al. (2024). Advances in Breast Cancer Prevention. ASCO Proceedings.
2. Johnson, L. et al. (2024). Lifestyle Factors in Cancer Prevention. ESMO Abstracts.
3. Brown, A. et al. (2024). AI in Cancer Diagnostics. ASCO Symposium.
4. Davis, R. et al. (2024). Liquid Biopsies in Oncology. ESMO Highlights.
5. Lee, C. et al. (2024). Molecular Heterogeneity of Breast Cancer. ASCO Reports.
6. Patel, M. et al. (2024). Genetic Markers in Breast Cancer. ESMO Presentations.
7. Wilson, H. et al. (2024). Innovations in Breast Cancer Surgery. ASCO Updates.
8. Garcia, F. et al. (2024). Advances in Radiation Therapy. ESMO Sessions.
9. Thompson, D. et al. (2024). Hormone Therapy Developments. ASCO Discussions.
10. Martinez, J. et al. (2024). CDK4/6 Inhibitors in Breast Cancer. ESMO Findings.
11. Nguyen, P. et al. (2024). Chemotherapy Agents and Protocols. ASCO Analysis.
12. Kim, S. et al. (2024). Combination Chemotherapy Regimens. ESMO Insights.
13. Chen, Y. et al. (2024). Checkpoint Inhibitors in Breast Cancer. ASCO Review.
14. Zhao, L. et al. (2024). Immunotherapy Combinations in Oncology. ESMO Reports.
15. Wang, X. et al. (2024). Role of Bevacizumab in Breast Cancer. ASCO Review.
16. Zhang, T. et al. (2024). HER2-Targeted Therapies: Advances and Challenges. ESMO Insights.
17. Liu, Y. et al. (2024). Antibody-Drug Conjugates in Breast Cancer. ASCO Highlights.
18. Zhao, L. et al. (2024). Vaccine Development in Breast Cancer. ESMO Reports.