Today is World Ovarian Cancer Day
- netmd
- 8 de mayo de 2024
- Oncología Médica
- 0 Comments
Adrian P. Hunis MD
Introduction
Today is World Ovarian Cancer Day. It is observed annually on May 8th with the aim of raising awareness about ovarian cancer and promoting education on the disease, as well as supporting affected women and their families.
Incidence
The worldwide incidence and mortality rates of ovarian cancer vary by region and over time. According to the World Health Organization (WHO), ovarian cancer is the 8th most common cancer in women worldwide, with an estimated 313,959 new cases and 207,252 deaths in 2020. The incidence and mortality rates can be influenced by factors such as access to healthcare, screening programs, lifestyle choices, and genetic predisposition. It is important to raise awareness about ovarian cancer and promote early detection and treatment to improve outcomes for women affected by this disease.
Risk factors for ovarian cancer include:
- Age: The risk of ovarian cancer increases with age, with most cases occurring in women over the age of 50.
- Family history: Women with a family history of ovarian, breast, or colorectal cancer may have an increased risk of developing ovarian cancer.
- Inherited genetic mutations: Mutations in genes such as BRCA1 and BRCA2 increase the risk of ovarian cancer.
- Personal history: A personal history of breast, uterine, or colorectal cancer may also increase the risk of ovarian cancer.
- Reproductive factors: Factors such as never having been pregnant, early onset of menstruation, and late onset of menopause may increase the risk of ovarian cancer.
- Hormone replacement therapy: Long-term use of hormone replacement therapy may increase the risk of ovarian cancer.
- Obesity: Being overweight or obese may be a risk factor for ovarian cancer.
- Endometriosis: Women with endometriosis have an increased risk of developing ovarian cancer.
- Use of fertility treatments: Some studies suggest that certain fertility treatments may increase the risk of ovarian cancer.
- Lifestyle factors: Factors such as smoking, alcohol consumption, and a diet high in fat may also increase the risk of ovarian cancer.
It is important to note that having one or more risk factors does not mean that a person will definitely develop ovarian cancer. Conversely, some women who develop ovarian cancer may not have any known risk factors. Regular screenings and early detection are key in managing the risk of ovarian cancer.
Advances in molecular studies
Advances in molecular studies in ovarian cancer have significantly improved our understanding of the disease and have led to the development of targeted therapies and personalized treatment approaches. Some key advances in molecular research in ovarian cancer include:
- Identification of genetic mutations: Studies have identified several genetic mutations, such as BRCA1 and BRCA2, that play a significant role in the development of ovarian cancer. Understanding these mutations has led to targeted therapies, such as PARP inhibitors, that specifically target cancer cells with these mutations.
- Genomic profiling: Advances in genomic sequencing technologies have allowed researchers to analyze the genetic makeup of ovarian tumors in detail. This has led to the identification of specific molecular subtypes of ovarian cancer, each with unique characteristics and potential treatment options.
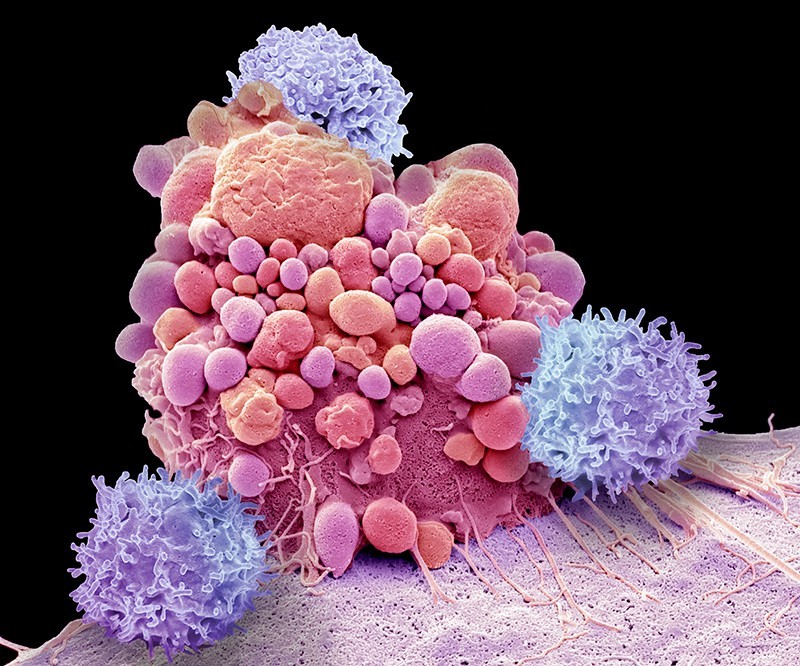
- Tumor microenvironment studies: Research on the tumor microenvironment, including interactions between cancer cells and surrounding stromal cells, immune cells, and blood vessels, has provided insights into the mechanisms of tumor growth and spread. This knowledge has led to the development of immunotherapies and targeted therapies that aim to disrupt these interactions and inhibit tumor growth.
- Liquid biopsy techniques: Liquid biopsy methods, such as circulating tumor DNA analysis, have emerged as non-invasive tools for monitoring disease progression, detecting resistance to treatment, and identifying potential therapeutic targets in ovarian cancer.
- Biomarker discovery: Ongoing research efforts have focused on identifying biomarkers that can predict treatment response, disease recurrence, and overall prognosis in ovarian cancer. These biomarkers have the potential to guide treatment decisions and improve patient outcomes.
Overall, molecular studies in ovarian cancer have greatly advanced our knowledge of the disease and have paved the way for personalized treatment approaches that target specific molecular alterations in individual patients. Continued research in this field holds promise for further improving outcomes for women with ovarian cancer.
The clinical aspects of ovarian cancer
refer to the medical and healthcare-related considerations and practices associated with the diagnosis, treatment, and management of ovarian cancer. This includes aspects such as symptoms and signs of the disease, diagnostic methods (such as imaging tests and biopsies), treatment options (such as surgery, chemotherapy, and targeted therapy), follow-up care, and supportive care to help manage symptoms and improve quality of life for patients with ovarian cancer. The clinical management of ovarian cancer involves a multidisciplinary approach, with healthcare providers from various specialties working together to provide comprehensive and personalized care for each patient.
Signs and symptoms
Refer to the physical manifestations and indications of a disease or condition that a person may experience. In the case of ovarian cancer, signs and symptoms can vary but may include abdominal bloating or swelling, pelvic or abdominal pain, difficulty eating or feeling full quickly, urinary symptoms (such as frequent urination), and changes in bowel habits. It is important for individuals to be aware of these signs and symptoms and to seek medical attention if they experience any persistent or concerning symptoms, as early detection and treatment can improve outcomes for ovarian cancer.
The diagnostic methods used for ovarian cancer may include:
- Imaging tests: such as ultrasound, CT scans, MRI scans, and PET scans to visualize the ovaries and surrounding tissues.
- Blood tests: such as CA-125 (a tumor marker) and other biomarker tests to assess for the presence of ovarian cancer.
- Biopsy: a tissue sample is taken and examined under a microscope to determine if cancer cells are present.
- Laparoscopy: a minimally invasive surgical procedure where a thin, lighted tube is inserted into the abdomen to view the ovaries and collect tissue samples.
These diagnostic methods are used to confirm the presence of ovarian cancer, determine the stage of the disease, and guide treatment decisions.
TNM and stages
The TNM staging system for ovarian cancer categorizes the extent of the primary tumor (T), regional lymph node involvement (N), and distant metastasis (M). The TNM staging system is commonly used to determine the stage of cancer and guide treatment decisions.
The staging of ovarian cancer is classified into four main stages, which are designated by Roman numerals I to IV. These stages are further subdivided into subcategories based on the extent of tumor spread. Here is how the stages of ovarian cancer are classified in:
– Stage I: Cancer is confined to the ovaries.
– Stage IA: Cancer is limited to one ovary.
– Stage IB: Cancer is present in both ovaries.
– Stage IC: Cancer is present in one or both ovaries with tumor on the surface of the ovary, capsule ruptured, or malignant cells in ascites or peritoneal washings.
– Stage II: Cancer has spread to other pelvic organs.
– Stage IIA: Cancer has spread to the uterus or fallopian tubes.
– Stage IIB: Cancer has spread to other pelvic organs.
– Stage IIC: Cancer has spread to pelvic organs with tumor on the surface of the ovary, capsule ruptured, or malignant cells in ascites or peritoneal washings.
– Stage III: Cancer has spread beyond the pelvis but is still within the abdominal cavity.
– Stage IIIA: Cancer has spread to the peritoneum outside the pelvis and/or regional lymph nodes.
– Stage IIIB: Cancer has spread to the peritoneum outside the pelvis and/or retroperitoneal lymph nodes.
– Stage IIIC: Cancer has spread to the peritoneum outside the pelvis and/or positive retroperitoneal lymph nodes.
– Stage IV: Cancer has spread to distant organs, such as the liver, lungs, or bones.
The TNM staging system and the classification of stages provide important information about the extent of the disease and help determine the most appropriate treatment approach for ovarian cancer patients.
The treatments for ovarian cancer may include:
- Surgery: The primary treatment for ovarian cancer is typically surgery to remove the tumor and any affected tissues, such as the ovaries, fallopian tubes, and nearby lymph nodes.
- Chemotherapy: Drugs are used to kill cancer cells or stop their growth, and chemotherapy is often used after surgery to kill any remaining cancer cells.
- Targeted therapy: Drugs that target specific molecules involved in cancer growth may be used in combination with chemotherapy.
- Immunotherapy: This treatment uses the body’s immune system to help fight cancer cells.
- Hormone therapy: This may be used in certain cases where the cancer cells are hormone-sensitive.
- Radiation therapy: This treatment uses high-energy rays to kill cancer cells and is less commonly used for ovarian cancer.
The specific treatment plan for ovarian cancer depends on factors such as the stage of the cancer, the type of ovarian cancer, the patient’s overall health, and personal preferences.
ASCO Guidelines 2024
The U.S. Food and Drug Administration (FDA) has approved several chemotherapy regimens, immunotherapy agents, and vaccines for the treatment of ovarian cancer. Some of the approved treatments include:
- Chemotherapy:
– Carboplatin and paclitaxel are commonly used chemotherapy drugs for ovarian cancer.
– Other chemotherapy drugs such as liposomal doxorubicin, gemcitabine, and topotecan may also be used in certain cases.
- Immunotherapy:
– The FDA has approved the immune checkpoint inhibitor pembrolizumab for the treatment of ovarian cancer with specific genetic abnormalities.
– Atezolizumab in combination with bevacizumab is another immunotherapy option that has been approved for certain patients with advanced ovarian cancer.
– Nivolumab and ipilimumab may also be used in certain cases.
- Vaccines:
– The FDA has not approved any vaccines specifically for ovarian cancer at this time. Clinical trials are ongoing to evaluate the efficacy of cancer vaccines in the treatment of ovarian cancer.
Intraperitoneal chemotherapy
Intraperitoneal chemotherapy is a treatment method where chemotherapy drugs are delivered directly into the peritoneal cavity, which is the space within the abdomen that contains organs such as the stomach, liver, and intestines. This approach is used in the treatment of certain types of ovarian cancer, particularly in advanced stages.
The value of intraperitoneal chemotherapy lies in its ability to directly target cancer cells within the abdominal cavity, where ovarian cancer often spreads. This method can help increase the concentration of chemotherapy drugs in the affected area and improve treatment outcomes compared to systemic chemotherapy alone.
The process of intraperitoneal chemotherapy involves a surgical procedure called intraperitoneal port placement, where a catheter is inserted into the peritoneal cavity. Chemotherapy drugs are then infused through the catheter, allowing for direct delivery to the affected area. The drugs may be administered on a specific schedule, often in combination with systemic chemotherapy for comprehensive treatment.
It is important to discuss the potential benefits and risks of intraperitoneal chemotherapy with a healthcare provider to determine if this treatment approach is appropriate for an individual’s specific situation.
New drugs
Some of the new drugs being investigated for the treatment of ovarian cancer include:
- Niraparib: Niraparib is a PARP inhibitor that has been approved for the maintenance treatment of recurrent ovarian cancer. It works by targeting DNA repair mechanisms in cancer cells.
- Bevacizumab: Bevacizumab is a monoclonal antibody that targets a protein called VEGF, which is involved in the growth of blood vessels that supply tumors. It is used in combination with chemotherapy for the treatment of advanced ovarian cancer.
- Olaparib: Olaparib is another PARP inhibitor that has been approved for the treatment of ovarian cancer with specific genetic mutations, such as BRCA mutations.
- Pembrolizumab: Pembrolizumab is an immune checkpoint inhibitor that has shown promising results in certain types of ovarian cancer, particularly those with specific genetic abnormalities.
- Rucaparib: Rucaparib is another PARP inhibitor that has been approved for the treatment of ovarian cancer in patients with certain genetic mutations.
These new drugs represent advancements in targeted therapies and immunotherapies for ovarian cancer and have the potential to improve outcomes for patients with this disease. It is important to consult with healthcare providers to determine the most appropriate treatment options based on individual factors and the latest advancements in ovarian cancer treatment.
Future
The future of ovarian cancer treatment looks promising with ongoing advancements in research and technology. Some potential areas of development and focus for the future of ovarian cancer treatment include:
- Personalized medicine: Tailoring treatment plans based on the individual genetic makeup of the tumor, allowing for more targeted and effective therapies.
- Immunotherapy: Expanding the use of immunotherapy agents and combination therapies to enhance the body’s immune response against ovarian cancer cells.
- Early detection methods: Developing improved screening tests and biomarkers for early detection of ovarian cancer, when treatment outcomes are typically better.
- Targeted therapies: Identifying new molecular targets and developing drugs that specifically target these pathways to inhibit cancer cell growth and survival.
- Precision medicine: Utilizing data from genetic profiling, molecular characterization, and other factors to guide treatment decisions and optimize outcomes for patients with ovarian cancer.
Overall, the future of ovarian cancer treatment is likely to continue moving towards more personalized, targeted, and effective therapies that aim to improve survival rates, quality of life, and overall outcomes for individuals diagnosed with this disease. Continued research, clinical trials, and collaboration among researchers, healthcare providers, and patients will be essential in advancing the field of ovarian cancer treatment.
Conclusions
In conclusion, ovarian cancer remains a significant health concern worldwide, but there have been notable advancements in understanding the disease, diagnosing it earlier, and developing more effective treatment options. Molecular profiling and genetic testing have opened up new possibilities for personalized medicine approaches, allowing for targeted therapies that can improve outcomes for patients with ovarian cancer. Clinical trials investigating chemotherapy, immunotherapy, and novel drugs are ongoing, offering hope for the future of ovarian cancer treatment.
It is essential for healthcare providers, researchers, and patients to continue working together to further advance the field of ovarian cancer treatment, improve early detection methods, and enhance patient outcomes. By staying informed about the latest developments in ovarian cancer research and treatment, individuals can make more informed decisions about their care and contribute to ongoing efforts to combat this disease. With continued progress and collaboration, the outlook for individuals affected by ovarian cancer is likely to improve in the years to come
References
- Armstrong, D. K., Alvarez, R. D., Bakkum-Gamez, J. N., Barroilhet, L., Behbakht, K., Berchuck, A., … & Dorigo, O. (2019). Ovarian cancer, version 2.2020, NCCN clinical practice guidelines in oncology. Journal of the National Comprehensive Cancer Network, 17(8), 896-909.
- Bowtell, D. D., Böhm, S., Ahmed, A. A., Aspuria, P. J., Bast, R. C., Beral, V., … & Coleman, R. L. (2015). Rethinking ovarian cancer II: Reducing mortality from high-grade serous ovarian cancer. Nature Reviews Cancer, 15(11), 668-679.
- Coleman, R. L., Fleming, G. F., Brady, M. F., Swisher, E. M., Steffensen, K. D., Friedlander, M., … & Santin, A. D. (2019). Veliparib with first-line chemotherapy and as maintenance therapy in ovarian cancer. New England Journal of Medicine, 381(25), 2403-2415.
- Kurman, R. J., & Shih, I. M. (2011). The origin and pathogenesis of epithelial ovarian cancer: a proposed unifying theory. The American Journal of Surgical Pathology, 34(3), 433-443.
- Matulonis, U. A., Sood, A. K., Fallowfield, L., Howitt, B. E., Sehouli, J., Karlan, B. Y., … & Hood, L. (2016). Ovarian cancer. Nature Reviews Disease Primers, 2(1), 16061.
- Ledermann, J. A., Raja, F. A., Fotopoulou, C., & Gonzalez-Martin, A. (2013). Newly diagnosed and relapsed epithelial ovarian carcinoma: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Annals of Oncology, 24(Supplement 6), vi24-vi32.
- Lheureux, S., Gourley, C., Vergote, I., Oza, A. M., & Epithelial Ovarian Cancer Task Force of the Gynecologic Cancer InterGroup. (2019). Epithelial ovarian cancer. The Lancet, 393(10177), 1240-1253.
- Prat, J. (2012). Ovarian carcinomas: five distinct diseases with different origins, genetic alterations, and clinicopathological features. Virchows Archiv, 460(3), 237-249.
- Vaughan, S., Coward, J. I., Bast, R. C., Berchuck, A., Berek, J. S., Brenton, J. D., … & Bowtell, D. D. (2011). Rethinking ovarian cancer: recommendations for improving outcomes. Nature Reviews Cancer, 11(10), 719-725.
- Vargas, A. N., & Natanzon, Y. (2020). Ovarian Cancer. In StatPearls [Internet]. StatPearls Publishing.
- Kossaï, M., Leary, A., Scoazec, J. Y., Genestie, C., & Ovarian Cancer Biomarkers: Current State and Future Implications from High-Throughput Technologies. Biomarkers in Cancer, 9, 1179299X17745955.
- Banerjee, S., & Kaye, S. B. (2013). New strategies in the treatment of ovarian cancer: current clinical perspectives and future potential. Clinical Cancer Research, 19(5), 961-968.
- Bowtell, D. D., & Brenton, J. D. (2010). Beyond genomics: understanding heterogeneity in high-grade serous ovarian cancer. Annals of Oncology, 24(Supplement 10), x7-x11.
- du Bois, A., Reuss, A., Pujade-Lauraine, E., Harter, P., Ray-Coquard, I., Pfisterer, J., … & Sehouli, J. (2013). Role of surgical outcome as prognostic factor in advanced epithelial ovarian cancer: a combined exploratory analysis of 3 prospectively randomized phase 3 multicenter trials: by the Arbeitsgemeinschaft Gynaekologische Onkologie Studiengruppe Ovarialkarzinom (AGO-OVAR) and the Groupe d’Investigateurs Nationaux Pour les Etudes des Cancers de l’Ovaire (GINECO). Cancer, 119(22), 4003-4011.
- Matulonis, U. A., & Horowitz, N. S. (2016). New developments in ovarian cancer screening and treatment. Cancer Journal, 22(5), 326-328.